The Other Silent Disease
Chronic kidney disease is often a “silent disease.”
Most patients just experience fatigue and low energy and often attribute these
symptoms to other things as opposed to a serious illness.
What are the needed improvements in kidney care?
- Earlier detection and treatment of CKD.
- Proactive education of patients with CKD to encourage a greater awareness of the disease and its consequences if left untreated.
- The provision of evidence-based care to slow down progression of CKD: focus on BP control, proteinuria; Hemoglobin A1C; smoking cessation.
- Intense patient education on their treatment options during stages 3-5.
- Optimization of the care they may be receiving as patients with end-stage kidney
disease.
Data from the 2020 Annual Data Report from the United States Renal Data System confirm that, of patients initiating dialysis for ESKD, more than 80% “crash” into dialysis during a hospital admission and end up initiating dialysis with a central venous catheter
and all its acute and chronic complications, including high risk of infection and.
Access when Initiating Dialysis
Source: 2020 USRDS Annual Data Report citing 2018 Vascular Access data
Prior nephrology care
Even patients who have been followed by a nephrologist prior to ESKD often do not know all their treatment options, such as transplantation, home dialysis and, importantly, conservative care as an alternative to in-center dialysis.
These “crashes” into in-center dialysis not only impact the patient’s health adversely, resulting in multiple hospitalization episodes and high mortality, but also result in high cost of care, whether the patient has private insurance, Medicare, or Medicaid. Rather than “crashing” into dialysis, patients with kidney disease should be empowered with knowledge and educated on ways they can slow down progression of their disease, learn about their treatment options when they progress to ESKD and help them prepare for whatever option they choose.
Alternative care models
The vision of Renal Care 360º is about raising awareness and knowledge of kidney disease in as many patients with CKD as possible and working with the medical community to raise the quality of care and patient satisfaction for patients with CKD and ESKD, resulting in better patient outcomes and cost efficiency in this expensive segment of health care.
The model of care is simple: repeatedly engage and talk with patients, preferably with face-to-face interactions with medical personnel.
Our interactions and educational program for patients follow three broad pathways that are complementary.
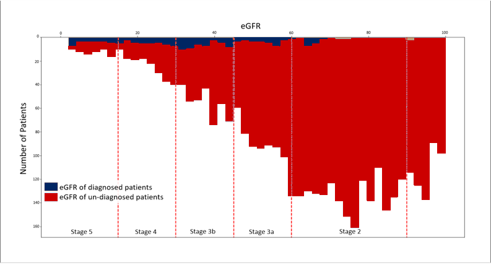
Focus on patients with eGFR from 60 mL/min/1.73 m2 to less than 20 mL/min/1.73 m.2 by educating patients about lifestyle changes that can slow down progression of their illness, such as the following:
- compliance with prescribed medications.
- avoidance of OTC nephrotoxic medications.
- monitoring and recording their BP daily and if they have diabetes monitor and record their blood sugar at least a few times daily to help their physician adjust their diabetes medication accordingly.
- diets that are rich in vegetables and fruits and low in sodium, phosphorus, and protein.
- Focus on educating patients with eGFR of less than 20 mL/min/1.73 m2 to make an informed decision for their ESKD treatment options, emphasizing transplant, home dialysis, self-care as options, but also in center therapy or conservative therapy.
- ESKD care-optimization program is aimed at patients with eGFR less than 15 mL/min/1.73 m2 who have or have begun to experience symptoms of kidney failure and for whom compliance with the right evidence-based treatment plan is critical. Again, the therapeutic options discussed are inclusive and consist of dialysis (with emphasis on home dialysis, transplantation preferably from a living related donor, or conservative therapy for patients who are at an older age (> 75 years) or have multiple comorbidities that may significantly reduce their well-being and the quality of their lifestyle if they are initiated on dialysis.
Patients Crashing Into Dialysis – A Comparison
Industry Average
RenalCare 360 Patients
Timely access placement
For those patients who elect dialysis as a modality choice, we discuss with them the need to prepare and initiate a timely access placement (AV fistula for those who elect hemodialysis and a PD catheter for those who elect the PD option), with emphasis on early placement of an AV fistula because they often require surgical revisions before the fistula matures and because placement of AV fistulas has been associated with improvement in eGFR.
We want to ensure patient compliance with an evidence-based pathway, be it conservative kidney care, transplant, or post-transplant care. For those on dialysis, we emphasize the need for treatment compliance.
Multidisciplinary care team
While most of these discussions with patients are performed by experienced nurses and advanced healthcare providers in the locality where patients live. Social workers and dieticians who can provide the patient with emotional support, particularly those with evident depression or denial of their health status and, for those who need it, help with transportation to medical entities or help them apply for external financial support.

When appropriate, patients with CKD (especially when the eGFR <30 mL/min/1.73 m2) who are not followed by a nephrologist are referred to the nephrology practice engaged with Renal Care 360, to receive their nephrology-specific care.
Our model of care is simple, and it is effective. We want to engage with patients referred or identified by a health plan or system as having CKD. We want to slow the progression of CKD through intense education and control of risk factors through evidence-based
care. For those patients who need to initiate dialysis we want to avoid “crashing” into dialysis and initiate planned dialysis, preferably initiating home dialysis. This will result in a significant decline in hospitalizations and re-hospitalizations.
About Dr. Steven Bander, M.D.
Dr. Bander is a well published expert and thought leader in both nephrology and vascular access. Currently, working in St. Louis, MO specializing in Nephrology and Interventional Nephrology with St. Luke’s Hospital as Medical Director of the Vascular Access Center.
Dr. Bander is considered an expert regarding all aspects of dialysis and has lectured and published both nationally and internationally on the topic of kidney care.






